Amnisure
Preterm premature rupture of membranes (PPROM) refers to rupture of fetal membranes prior to labor in pregnancies of less than 37 weeks. It occurs in 3 percent of pregnancies and is responsible for one-third of preterm births. A history of PPROM, genital tract infection, antepartum bleeding, and cigarette smoking are risk factors for PPROM. Complications of PPROM include maternal and neonatal infection, preterm delivery, abruptio placenta, and cord prolapse. The classic clinical presentation of PPROM is a sudden gush of clear or pale yellow fluid from the vagina. However, many women describe intermittent or constant leakage of small volumes of fluid or a sensation of wetness within the vagina or perineum. A clinical history suggestive of PPROM should be confirmed by visual inspection or laboratory tests to exclude other causes of wetness, such as urinary incontinence, vaginal discharge, and perspiration.
The best method of confirming the diagnosis of PPROM is direct observation of amniotic fluid coming out of the cervical canal or pooling in the vaginal fornix. If PPROM is not obvious after visual inspection, the diagnosis can be confirmed by testing the pH of the vaginal fluid, which is easily accomplished with nitrazine paper. Amniotic fluid has a pH range of 7.0 to 7.7 compared to the normally acidic vaginal pH of 3.8 to 4.2 (Seeds, AE, Hellegers, AE. Acid-base determinations in human amniotic fluid throughout pregnancy. Am J Obstet Gynecol 1968; 101:257).
False-negative and false-positive test results occur in up to 5 percent of cases (Abe, T. The detection of rupture of fetal membranes with the nitrazine indicator. Am J Obstet Gynecol 1940; 39:400 and Davidson, KM. Detection of premature rupture of the membranes. Clin Obstet Gynecol 1991; 34:715). False negative tests results can occur when leaking is intermittent or the amniotic fluid is diluted by other vaginal fluids. False positive results can be due to the presence of alkaline fluids in the vagina, such as blood, seminal fluid, soap, or some infections.
Another confirmatory test is the presence of arborization (ferning). Fluid from the posterior vaginal fornix is swabbed onto a glass slide and allowed to dry for at least 10 minutes. Amniotic fluid produces a delicate ferning pattern, in contrast to the thick and wide arborization pattern of dried cervical mucus. Well-estrogenized cervical mucus or a fingerprint on the microscope slide may cause a false-positive fern test; false negatives can be due to inadequate amniotic fluid on the swab or heavy contamination with vaginal discharge or blood.
The newest confirmatory test is the AmniSure®, which is a point of care immunochromatographic assay that detects trace amounts of placental alpha microglobulin-1 protein (PAMG-1) in vaginal fluid after rupture of fetal membranes. The analytical sensitivity of the test has been set at 5 ng/mL. PAMG-1 is not detected when fetal membranes are intact because the concentration of PAMG-1 in cervical vaginal secretions is less than 0.25 ng/mL. AmniSure® assay does not require a speculum examination. Amnisure is approved by FDA for use at any gestational age.
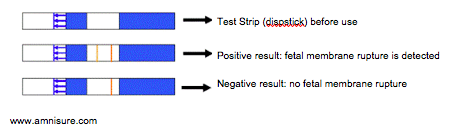
A sterile swab is inserted into the vagina for one minute and then placed into a vial containing a solvent that extracts protein from the swab. After one minute, an AmniSure test strip is dipped into the vial. The pad region of the test strip contains soluble murine monoclonal antibody to PAMG-1 that is conjugated with colloidal gold particles. These antibodies bind to PAMG-1, if it is present. The antigen-antibody complex migrates to the test region of the strip, which contains solid phase rabbit anti-mouse antibody that captures PAMG-1 antibody complexes flowing up from the Pad Region. After five to ten minutes, immobilized colloidal gold conjugated PAMG-1 produces a brown/yellow stripe in the test region. A second stripe in the control region indicates that the test strip functioned properly. This stripe appears when rabbit anti-mouse IgG antibody catches the mouse A-antibody with dye gold. One visible line means a negative result for amniotic fluid, two visible lines is a positive result, no visible lines is an invalid result).
Two large studies have assessed the efficacy of AmniSure®. In a study of 203 gravidas suspected of ruptured membranes, the sensitivity and specificity of the AmniSure device were 98.9 and 100 percent, respectively (Cousins, LM, Smok, DP, Lovett, SM, Poeltler, DM. AmniSure placental alpha microglobulin-1 rapid immunoassay versus standard diagnostic methods for detection of rupture of membranes. Am J Perinatol 2005; 22:317). Test performance was calculated by comparing AmniSure results against clinical history, nitrazine and fern results, presence of pooling, sonographic evidence of oligohydramnios, and findings from repeated examinations.
Another study of 184 gravidas suspected of ruptured membranes reported the sensitivity and specificity of the AmniSure device were 98.7 and 87.5 percent, respectively (Lee, SE, Park, JS, Norwitz, ER, et al. Measurement of placental alpha-microglobulin-1 in cervicovaginal discharge to diagnose rupture of membranes. Obstet Gynecol 2007; 109:634). Test performance was calculated similar to the first study. The cause of false positive results in three patients was unknown; the possibility of a small leak of amniotic fluid that sealed over could not be excluded.
A false positive result may occur in the case of bleeding in a woman with a pathological pregnancy. Conducting the test when there is a discharge of blood is not recommended. A small amount of blood admixture in the sample does not interfere with test results.
A false negative result may occur when the sample is taken 12 or more hours after a presumed fetal membrane rupture has occurred. Amnisure is not affected by a hight dose hook effect. AmniSure® should not be used within 6 hours after the removal of any disinfectant solutions or medicines from the vagina.


